In this first blog for 2022, we will be looking to raise awareness around Cervical Cancer and how it affects minorities as part of the Cervical Cancer awareness month. Innovative Trials are passionate about ensuring our diverse population is adequately represented within medical research. Whether it is wanting to see more people from underrepresented communities choosing science as a career and pushing for greater patient diversity in clinical trials or focusing on what we are doing internally to celebrate and promote equality and diversity. Throughout 2021, we have made a pledge to share our education and experiences with our clients and colleagues, to ensure inclusivity across the board. Each month we will be releasing communications in line with national and international awareness campaigns. In 2021, we have explored: Women’s Health; diversity in Cancer, Heart Disease and Scleroderma, Ovarian and Prostate Cancer, Autism Acceptance,Ramadan and Bowel Cancer, Stroke and Hepatitis, Mental Health, Pride month, Women with Alopecia, Psoriasis, Dementia, Disability , Black History Month and Lupus
Introduction 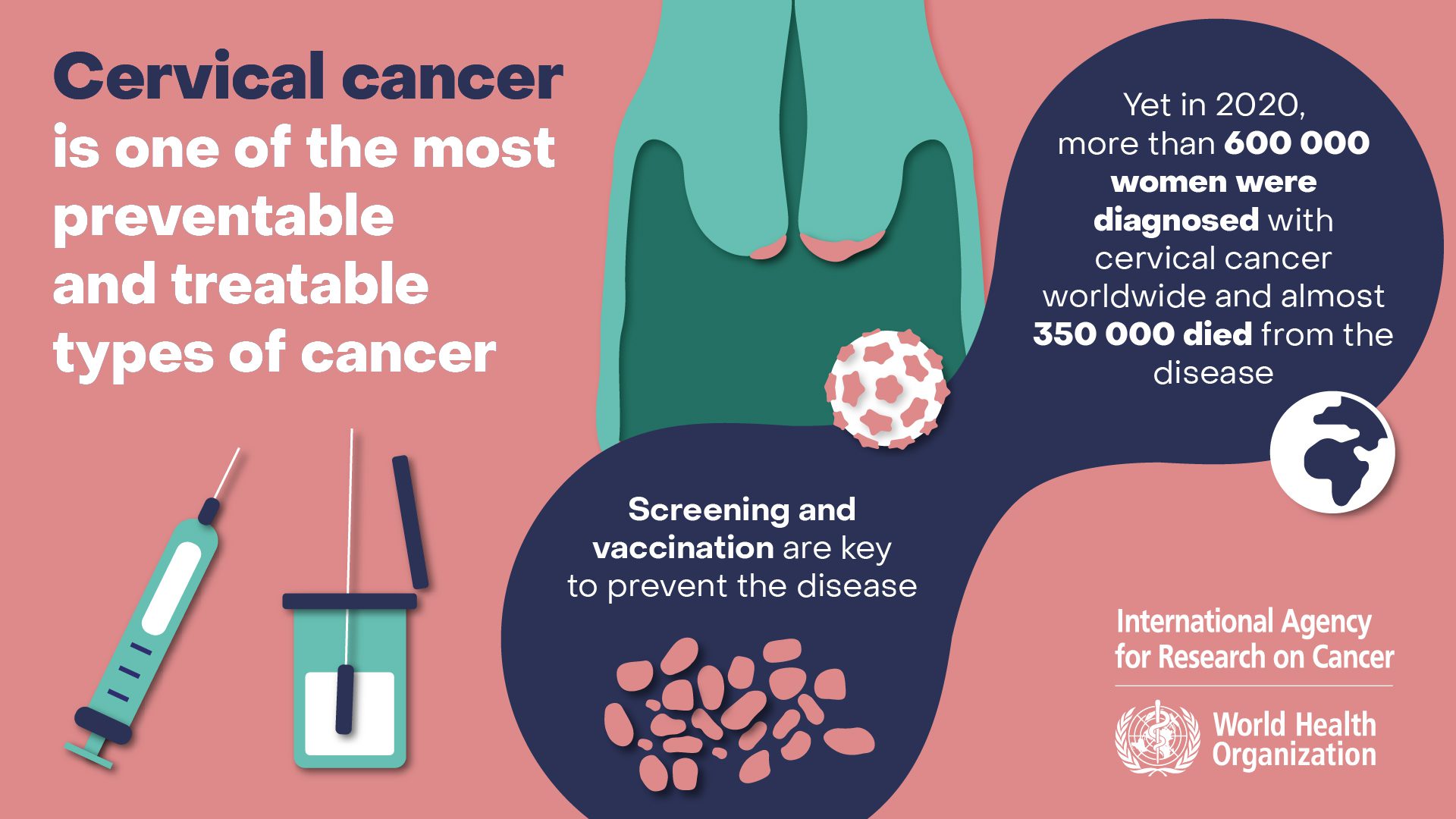 Every year in the UK, around 3,200 women are diagnosed with cervical cancer (around 9 every day) with about 850 deaths from the disease (around 2 every day). It is a cancer that affects younger people disproportionately, with more than half of those diagnosed under the age of 45 (Cancer Research UK 2016-2018). In 2020, an estimated 604,000 women were diagnosed with cervical cancer worldwide, 342,000 of whom died from the disease (UN News, 5 January 2022). Despite cervical cancer incidence decreasing by 25% in the UK since the 1990’s, these figures could be dramatically improved upon as 99.8% cases are preventable (Cancer Research UK 2016-2018). World Health Organization (WHO) chief Tedros Adhanom Ghebreyesus tweeted, saying “it could be the first cancer EVER to be eliminated” (UN News, 5 January 2022). This is a bold claim but one that could be realised. 17-23 January is Cervical Cancer Prevention Week, so let’s raise awareness on how to make this happen! How Can You Help Prevent Cervical Cancer?
Every year in the UK, around 3,200 women are diagnosed with cervical cancer (around 9 every day) with about 850 deaths from the disease (around 2 every day). It is a cancer that affects younger people disproportionately, with more than half of those diagnosed under the age of 45 (Cancer Research UK 2016-2018). In 2020, an estimated 604,000 women were diagnosed with cervical cancer worldwide, 342,000 of whom died from the disease (UN News, 5 January 2022). Despite cervical cancer incidence decreasing by 25% in the UK since the 1990’s, these figures could be dramatically improved upon as 99.8% cases are preventable (Cancer Research UK 2016-2018). World Health Organization (WHO) chief Tedros Adhanom Ghebreyesus tweeted, saying “it could be the first cancer EVER to be eliminated” (UN News, 5 January 2022). This is a bold claim but one that could be realised. 17-23 January is Cervical Cancer Prevention Week, so let’s raise awareness on how to make this happen! How Can You Help Prevent Cervical Cancer?
- Having the HPV vaccination if aged 12-18 years
- Attending cervical screening when invited
- Familiarising yourself with the the symptoms of cervical cancer and seeking the right medical advice and support for them
What is HPV? HPV stands for Human Papillomavirus: The name of a very common group of viruses (most people will get some type of HPV in their lives). Mostly, they are relatively harmless, but some types can cause genital warts or cancer (of which cervical cancer is one). A common misconception is that you must have had penetrative sex to catch HPV. However, this is not the case as you can catch it from any skin-to-skin contact of the genital area or sharing sex toys (NHS 19 March 2019). Virtually all cervical cancers are caused by HPV. However, there is an HPV vaccine that is available for girls and boys aged 12-18 years. It is given to people at such a young age as it is more effective before young people take part in any sexual activity where the virus could be spread. 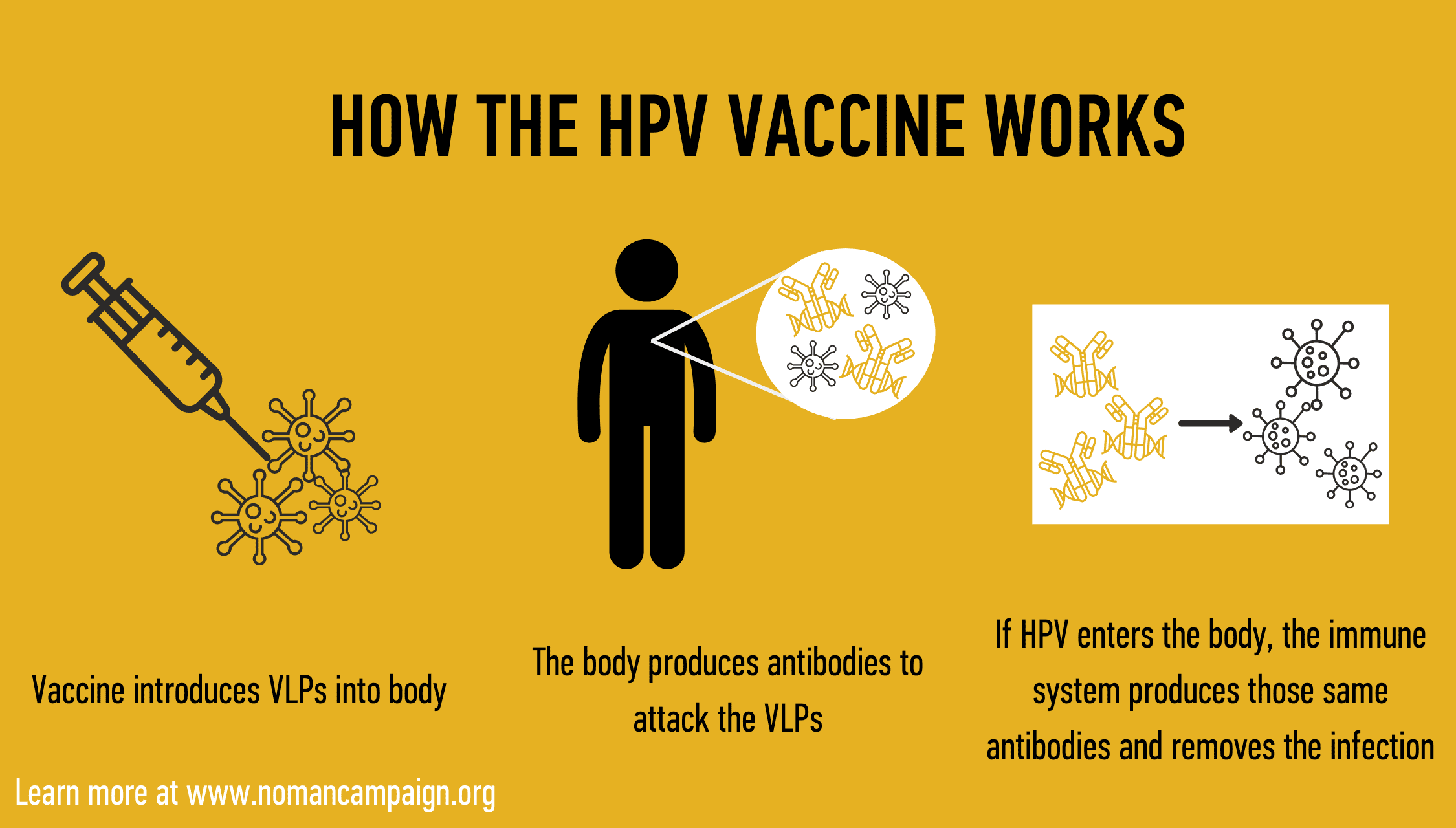
HPV Immunisation Programme
The programme was launched in England 13 years ago and a recent study showed that it has so far prevented cervical cancer developing in thousands of women. It reported that vaccinating girls against HPV, has dramatically reduced the rates of cervical cancer in women (Falcaro M et al, 2021). They found that cervical cancer rates were 87% lower in women who were vaccinated against HPV when they were between ages 12 and 13 compared to previous generations. The rate of cervical cancer in women who were vaccinated between ages 14 and 16 was 62% lower. And in those vaccinated between 16 and 18, it was 34% lower.
What is the Cervical Screening Program? Cervical screening (also known as a smear test) checks the health of your cervix. The sample is checked for certain types of HPV and if these ‘high risk’ types of HPV are found then the sample is analysed for any changes to the cells of the cervix. These can then be treated, preventing them turning into cervical cancer. (Public Health England, 17 March 2021). The screening programme invites all women from age 25 to 64 for screening. Across the UK, cervical screening attendance has been falling. Factors that have contributed to this include difficulty getting appointments, embarrassment and lack of time. Coronavirus has undoubtedly had an impact on this, with fewer appointments available and lots of uncertainty about attending cervical screening during the pandemic. One solution to this is to provide the option to self-sample from home, negating the need to attend a clinic and this is something that Jo’s Cervical Cancer Trust have pushed for for a long time. (Jo’s Cervical Cancer Trust, 13 January 2021). Self-sampling doesn’t require a speculum (as previously used in the clinic) but uses a swab (like a long cotton bud) or a soft brush to collect a sample from your vagina. Self-sampling enables socially distanced cervical screening and better-accesses hard-to-reach groups. As evidence mounts that self-sampling is at least equivalent to clinician-collected samples, the focus for self-sampling is now as a primary screening option for all women. The London study began in mid-January 2021 and, if it is successful, could mean that the national screening programmes will soon be able to offer self-sampling to all women. (Anita W W Lim, February, 2021). How to spot the symptoms of Cervical Cancer? Cervical cancer may not cause any symptoms, or the symptoms may not be obvious. The most common symptoms of cervical cancer include:
- vaginal bleeding that is unusual for you, including after the menopause, after sex, or between regular periods
- changes to vaginal discharge
- pain or discomfort during sex
- unexplained pain in your lower back or between your hip bones (pelvis).
It is important to remember that these symptoms usually happen for reasons other than cervical cancer. But it is also important to contact your GP straight away, so they can give you reassurance and support (Cancer Research UK 2016-2018). 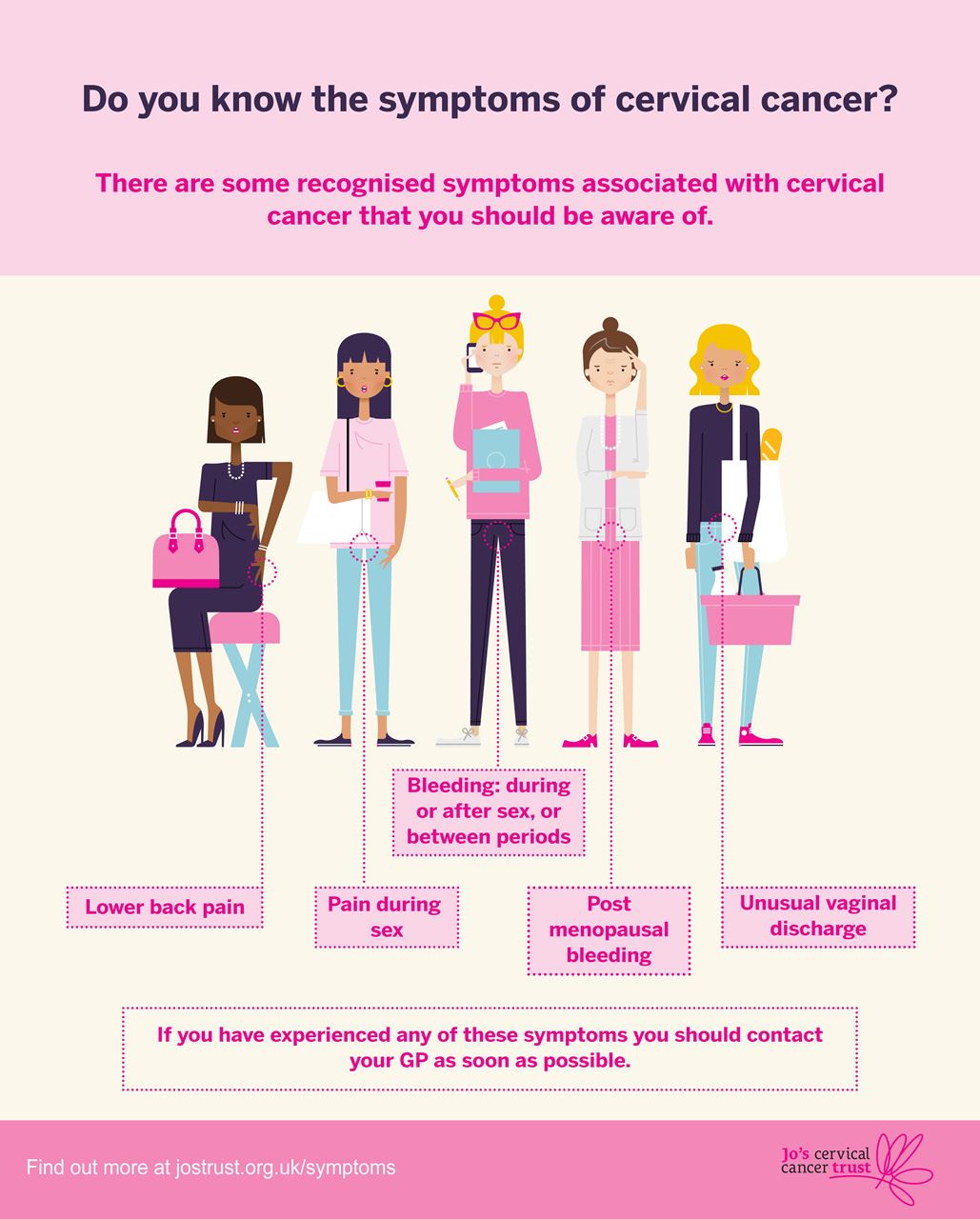 Inequalities The charity, Jo’s Cervical Cancer Trust, carried out a YouGov survey which revealed variation between BAME and white women in terms of attending screening, understanding the importance of cervical screening and knowledge about the test. For example, 12% of BAME women were more likely than white women (8%) to say they had never had a screening test and BAME women are twice as likely as white women to say that better knowledge about the test and of its importance would motivate them to be screened (Jo’s Cervical Cancer Trust, 2019). This has highlighted the need for further education within the BAME community on cervical cancer screening and its importance. In 2018, nearly 90% of deaths from cervical cancer were from low and middle-income countries. This is largely because access to public health services is limited and screening and treatment are not widely available. Because of this, IARC (International Agency for Research on Cancer) and WHO have united to develop an inclusive and ambitious strategy to prevent cervical cancer altogether (UN News, 5 January, 2022). This is called the Global Strategy for Elimination of Cervical Cancer and aims for each country to have the following targets by 2030:
Inequalities The charity, Jo’s Cervical Cancer Trust, carried out a YouGov survey which revealed variation between BAME and white women in terms of attending screening, understanding the importance of cervical screening and knowledge about the test. For example, 12% of BAME women were more likely than white women (8%) to say they had never had a screening test and BAME women are twice as likely as white women to say that better knowledge about the test and of its importance would motivate them to be screened (Jo’s Cervical Cancer Trust, 2019). This has highlighted the need for further education within the BAME community on cervical cancer screening and its importance. In 2018, nearly 90% of deaths from cervical cancer were from low and middle-income countries. This is largely because access to public health services is limited and screening and treatment are not widely available. Because of this, IARC (International Agency for Research on Cancer) and WHO have united to develop an inclusive and ambitious strategy to prevent cervical cancer altogether (UN News, 5 January, 2022). This is called the Global Strategy for Elimination of Cervical Cancer and aims for each country to have the following targets by 2030:
- 90% coverage of HPV vaccination of girls (by 15 years of age)
- 70% coverage of screening (70% of women screened with high-performance tests by the ages of 35 and 45 years)
- 90% treatment of precancerous lesions and management of 90% of invasive cancer cases
WHO is calling on all countries and partners to help eliminate cervical cancer within the next century. This is far more achievable than it may seem, providing awareness is raised and preventative steps are taken in every corner of the globe. If you need further support visit: https://www.macmillan.org.uk/cancer-information-and-support/diagnostic-tests/cervical-screening https://www.csas.nhs.uk/ https://twitter.com/i/status/1478369794848141320 https://youtu.be/72vgP2qtmW4 References
- Cancer Research UK cervical cancer statistics (2016-2018). Retrieved 8th January 2022, from https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer
- Falcaro M et al. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet2021;(Nov). doi:10.1016/S0140-6736(21)02178-4.
- Jo’s Cervical Cancer Trust. The differing understanding of cervical screening among white women and women from a Black, Asian and Minority Ethnic (BAME) community (9 July 2019). Retrieved 13th January 20222 from https://www.jostrust.org.uk/about-us/our-research-and-policy-work/our-research/cervical-screening-among-bame-communities
- Jo’s Cervical Cancer Trust (13 January 2021). Retrieved 9th January 20222 from. https://www.jostrust.org.uk/about-us/news-and-blog/blog/what-hpv-self-sampling
- Landy et al (2022). Non-speculum sampling approaches for cervical screening in older women: randomised controlled trial. Retrieved 10th January 2022 from https://bjgp.org/content/72/714/e26
- Anita WW Lim. Will COVID be the tipping point for primary HPV self-sampling? Retrieved 10th January 2021 from https://cebp.aacrjournals.org/content/30/2/245.abstract
- NHS (19 March 2019). Retrieved 8th January 2022 from https://www.nhs.uk/conditions/human-papilloma-virus-hpv/
- Public Health England (17 March 2021) NHS cervical screening programme(CSP). Retrieved 9th January 2022 from https://www.gov.uk/guidance/cervical-screening-programme-overview
- UN News, 5 January 2022. Retrieved 10th January 2022 from : https://news.un.org/en/story/2022/01/1109152
